Atrial fibrillation (AFib) affects the electrophysiology, or the function of the electrical system, in the heart and is the most common sustained arrhythmia (irregular heartbeat). If you have AFib, you may be referred to a type of heart specialist called an electrophysiologist. An electrophysiologist may recommend atrial fibrillation medications, lifestyle changes, and/or procedures such as an electrical cardioversion or a heart ablation to treat AFib episodes and prevent your next AFib attack.
In this post, our cardiologists in Colorado tackle some frequently asked questions regarding electrophysiology and AFib.
Does an electrophysiologist treat AFib?
 An electrophysiologist is a cardiologist who has attended a subspecialty fellowship training program that focuses specifically on the diagnosis and management of heart rhythm disorders and electrical problems in the heart.
An electrophysiologist is a cardiologist who has attended a subspecialty fellowship training program that focuses specifically on the diagnosis and management of heart rhythm disorders and electrical problems in the heart.
To become a board-certified electrophysiologist a person completes:
- 4 years of medical school
- 3 year of internal medicine training (residency)
- 3-4 years of training in disorders affecting the cardiovascular system
- 2 years of additional training in the diagnosis and management of conditions affecting the heart’s electrical system (electrophysiology)
If you have an arrhythmia, working with an electrophysiologist heart specialist can improve your outcomes and get you back to living the life you enjoy as soon as possible. Electrophysiologists are experts in treating the following arrhythmias:
- Supraventricular tachycardia. A sudden, rapid heartbeat caused by an abnormal pathway in the heart’s electrical system
- Atrial fibrillation. An irregular heartbeat caused by abnormal electrical signals in the upper heart chambers (atria)
- Atrial flutter. Abnormal heart rhythm caused by abnormal electrical signals in the atria.
- Bradycardia. The heart beats too slowly
- Tachycardia. The heart beats too fast
- Ventricular tachycardia. A dangerous abnormal heart rhythm
- Ventricular fibrillation. A dangerous irregular heartbeat that compromises the heart’s ability to pump blood to the body
- Channelopathies. Inherited cardiac channel diseases that interfere with the normal functioning of the heart’s electrical system
Because atrial fibrillation is the most common abnormal heart rhythm, electrophysiologist (EP) specialists care for patients with this condition on a daily basis and are the foremost experts on atrial fibrillation treatment.
What causes AFib to flare up?
 Atrial fibrillation begets atrial fibrillation. This means that if you have had atrial fibrillation, you are likely to have it again and the more frequently you have it, the more likely you are to stay in it for longer periods of time. The presence of certain AFib risk factors and triggers increase your chances of having another AFib attack.
Atrial fibrillation begets atrial fibrillation. This means that if you have had atrial fibrillation, you are likely to have it again and the more frequently you have it, the more likely you are to stay in it for longer periods of time. The presence of certain AFib risk factors and triggers increase your chances of having another AFib attack.
AFib triggers include:
- Alcohol. While it is possible that moderate alcohol intake (up to 1 drink/day for women and 2 drinks/day for men) may have some heart protective effects, this is not the case if you have atrial fibrillation. Alcohol irritates the heart’s electrical system, particularly heavy alcohol consumption and binge drinking.
- Acute stress, anxiety, depression, or strong emotions, like anger
- Food triggers. AFib food triggers are highly individualized but some reported food triggers for an atrial fibrillation attack are caffeine, excess salt, and cold/frozen food, like ice cream.
- Smoking or using tobacco products
- Certain viral infections
- Serious illness or pneumonia
- Surgery
- Excess thyroid hormone
- Lung disease. Any condition that impacts the lungs’ ability to deliver oxygen to the blood will increase the risk of developing an irregular heartbeat, like atrial fibrillation or atrial flutter. Lung disease can be chronic, like COPD, or acute, like pneumonia or pulmonary embolism (blood clots in the lungs).
In addition to these triggers, not taking your medications as prescribed can have a negative effect on your AFib. This applies not only to your AFib medications but also to medications you take to treat AFib risk factors. Untreated or inadequately treated AFib risk factors can cause an AFib attack. Health conditions that have been linked to AFib include:
- High blood pressure (hypertension)
- Heart failure
- Diabetes
- Coronary artery disease and heart attack (myocardial infarction)
- Sleep apnea
- Chronic kidney disease
- Overactive thyroid (hyperthyroidism)
- Lung disease
- Heart valve disease
- Obesity
If you have any of these conditions, it is important to work closely with your healthcare provider to ensure you are optimizing treatment as this will not only make you healthier, it can also help prevent future AFib episodes or AFib disease progression.
How long is it OK to be in AFib?
While atrial fibrillation is generally not an emergency, the short answer to this question is that it is better to be in a normal rhythm than to be in AFib. We used to think that it was ok to be in AFib as long as the heart rate was controlled (i.e less than 100 beats per minute at rest). However, research has shown that people do better in the long run if they can be kept in a normal heart rhythm. Because atrial fibrillation causes the heart to work less effectively, it increases the risk of stroke and heart failure and often has a negative impact on a person’s quality of life.
How can an electrophysiologist help with atrial fibrillation?

Electrophysiologists are experts in heart-rhythm abnormalities and arrhythmia treatment. Heart rhythm (EP) specialists may recommend atrial fibrillation medications or catheter-based interventions, such as heart ablation, to manage your atrial fibrillation.
A catheter ablation is a common catheter-based intervention electrophysiologists perform to treat atrial fibrillation. Catheter ablations are very effective at treating paroxysmal (intermittent) atrial fibrillation. As AFib progresses to become persistent or chronic atrial fibrillation, it becomes more difficult to treat and catheter ablation becomes less effective. If you have persistent atrial fibrillation, an electrophysiologist may refer you to a cardiac surgeon for a surgical alation. While surgical ablation is very effective, it is also more invasive than catheter ablation and therefore carries with it a higher risk of complications.
The benefits of early rhythm control with catheter ablation are:
- Improved long-term cardiovascular outcomes
- Catheter ablation is more effective than arrhythmia medications at preventing AFib progression (i.e. paroxysmal to persistent or permanent AFib).
- Catheter ablation decreases the amount of time you spend in AFib (a.k.a. AFib burden)
- Early catheter ablation increases procedural effectiveness
- Early ablation decreases cardiovascular hospitalizations.
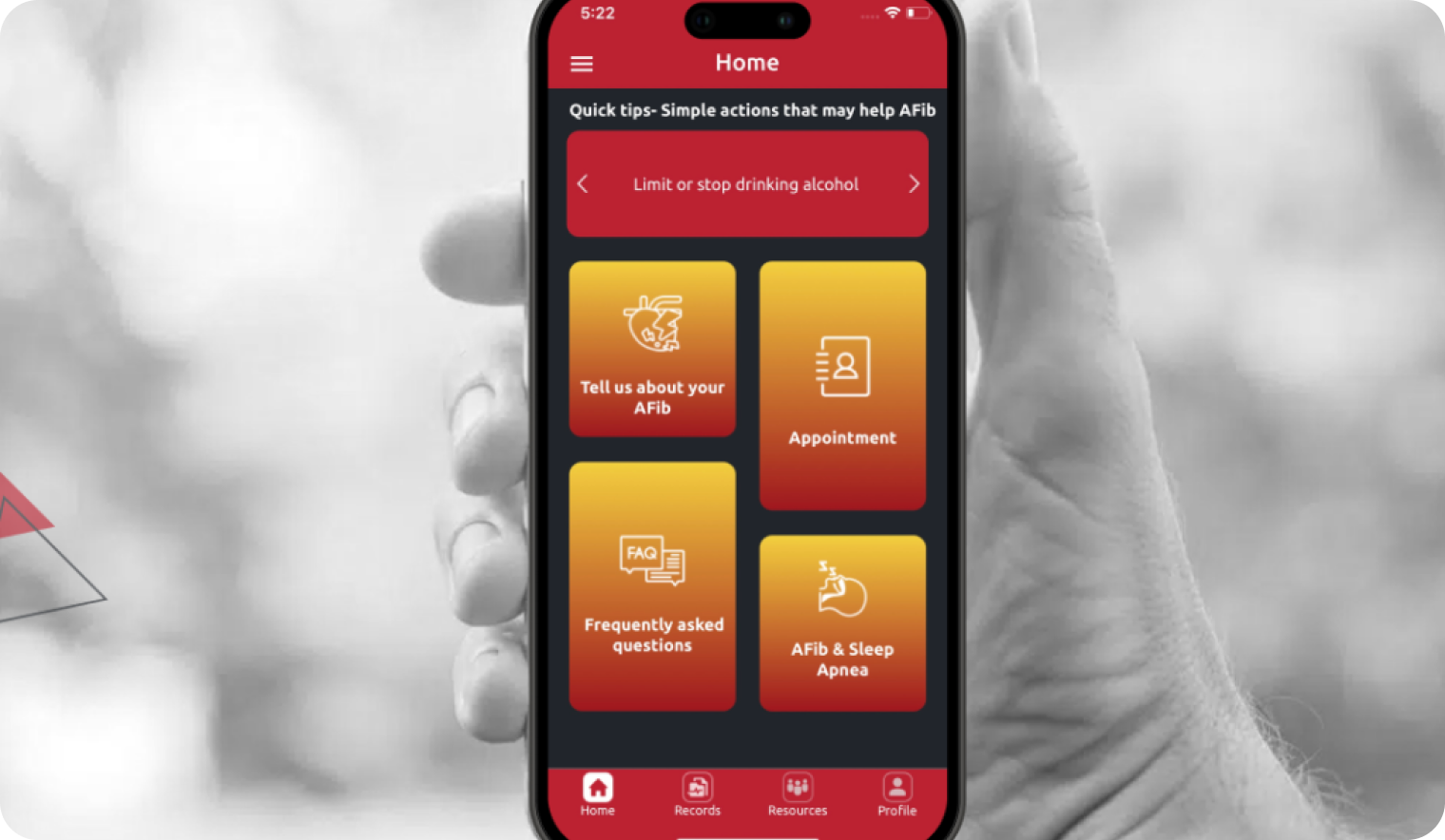
What questions should I ask an electrophysiologist?
General Questions
- What is causing my AFib?
- What type of AFib do I have?
- Do I have identifiable or modifiable AFib risk factors?
- Are there activities I should avoid?
- Are there lifestyle changes I could make to improve my chances of being AFib free?
Arrhythmia Treatment Questions
- Would it be better to treat my AFib with atrial fibrillation medications or a heart ablation?
- What are the side effects of the medications you are planning to prescribe? Is any routine monitoring required for any of the medication I will be taking?
- How many years have you been performing ablations? How many ablations do you perform each year?
- Am I a good candidate for catheter ablation for treatment of my atrial fibrillation (or atrial flutter)?
- Will having an ablation enable me to stop my atrial fibrillation medications?
- What type of ablation do you do (i.e. cryoablation, radiofrequency, laser ablation, etc)? Why do you prefer this technique?
- Will I be under general anesthesia or conscious sedation during the ablation?
- How long will I stay in the hospital after a catheter ablation?
- What is the recovery time after a catheter ablation?
- How frequently will I need to be seen after an ablation and who will I be seeing for these visits?
Stroke Prevention Questions
- What is my risk of having a stroke because of my AFib?
- What are my treatment options for reducing my stroke risk?
- Will I be able to stop my blood thinner (anticoagulation) if I undergo a procedure for stroke prevention?
What happens at the first electrophysiologist appointment?
 If you have atrial fibrillation, your primary care provider or cardiologist may refer you to an electrophysiologist. When you see the electrophysiologist, the heart specialist will perform an initial evaluation, physical exam, and recommend diagnostic tests. The following things may be done or discussed at your first visit with the electrophysiologist:
If you have atrial fibrillation, your primary care provider or cardiologist may refer you to an electrophysiologist. When you see the electrophysiologist, the heart specialist will perform an initial evaluation, physical exam, and recommend diagnostic tests. The following things may be done or discussed at your first visit with the electrophysiologist:
- Medical/surgical history and current medications. Take a list of any medications and supplements you are taking, including dose and frequency.
- Family history. People who have a family member with atrial fibrillation have a higher risk of developing AFib themselves.
- Arrhythmia treatment history. Knowing when you were diagnosed with AFib and what treatments have you tried will help the electrophysiologist develop your treatment plan. It can be helpful to write down any atrial fibrillation medications you have tried including why they were stopped. Also, bring a complete list of any AFib procedures (i.e. electrical cardioversion, catheter-based interventions, or surgical ablation) you have had.
- Diagnostic testing. In addition to the information you can provide about your health history, family history, and symptoms of AFib, the electrophysiologist will often order diagnostic tests to which will assist in AFib diagnosis and treatment. Diagnostic tests are also helpful in identifying underlying causes of atrial fibrillation. Your electrophysiologist may order some of the following tests:
- Blood work. This is done to check thyroid function, kidney function, electrolytes and check for abnormalities in the blood that could cause AFib.
- Electrocardiogram (EKG or ECG). A tracing of the heart’s electrical activity that allows your doctor to see the heart rhythm and rate.
- Echocardiogram. Ultrasound of the heart that allows your doctor to assess the structure and function of the heart.
- Heart monitor. A portable heart monitor you wear to help identify the type, frequency and duration of arrhythmias, such as AFib or atrial flutter.
- Stress test. Test to check for blockages in the arteries that feed the heart muscle (coronary artery disease) which could be contributing to your AFib.
- Chest X-ray. X-ray pictures of your heart and lungs.
- Sleep study. If you have symptoms that are concerning for sleep apnea, a sleep study may be ordered.
After the EP has reviewed the results of any diagnostic testing that was obtained, recommendations will be made regarding treatment options for your atrial fibrillation. The goal of AFib treatment is to maximize the time you spend in a normal heart rhythm, minimize AFib symptoms to improve your quality of life, and prevent stroke.
Sources
- Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020 Oct 1;383(14):1305-1316.
- Kuck KH, Lebedev ES, et al. Catheter ablation or medical therapy to delay progression of atrial fibrillation: the randomized controlled atrial fibrillation progression trial (ATTEST). EP Europace. March 2021; 23(3):362–369a.
- Blomström-Lundqvist C, Gizurarson S, Schwieler J, et al. Effect of catheter ablation vs antiarrhythmic medication on quality of life in patients with atrial fibrillation: The CAPTAF Randomized Clinical Trial. JAMA. 2019 Mar 19;321(11):1059-1068.
- Kawaji T, Shizuta S, et al. Early choice for catheter ablation reduced readmission in management of atrial fibrillation: Impact of diagnosis-to-ablation time. Int J of Cardio. 2019 Sept;291:69-76.